
People opposed to COVID-19 vaccines often embrace ivermectin, a drug they think is not getting the attention it deserves. Here, an anti-vaccination protester takes part in a rally against vaccine mandates last month in Santa Monica, Calif.
Ringo Chiu/AFP via Getty Images
hide caption
toggle caption
Ringo Chiu/AFP via Getty Images

People opposed to COVID-19 vaccines often embrace ivermectin, a drug they think is not getting the attention it deserves. Here, an anti-vaccination protester takes part in a rally against vaccine mandates last month in Santa Monica, Calif.
Ringo Chiu/AFP via Getty Images
Through July and August, Julie Smith watched her husband, Jeffrey, get worse and worse from COVID-19. In early July, the healthy outdoorsman, 51, had tested positive for the coronavirus. Within a week, he was admitted to the intensive care unit at a hospital near their home in the suburbs of Cincinnati.
The hospital treated him with antiviral drugs, convalescent plasma and steroids, but he continued to decline. Weeks later he was on a ventilator in a medically induced coma — “on death’s doorstep,” Julie Smith wrote in a legal complaint filed Aug. 20.
Smith felt the hospital had given up on her husband, but she could not, according to the complaint. After doing research on the internet, she sued the hospital to require it to treat her husband with ivermectin — an inexpensive anti-parasitic drug that’s been used to cure animals and people from worms and lice since the 1980s.
U.S. health authorities and most doctors do not recommend using it to prevent or treat COVID-19, citing a lack of clear evidence on whether the drug works. Yet myths and beliefs around the drug have taken on a life of their own, fueled by a small group of doctors whose views diverge from the medical consensus, by right-wing commentators and by internet groups where people share tips on sourcing and dosing.
That people such as Smith and a handful of other families of COVID-19 patients are turning to the courts to enforce treatment with the drug shows how heated the debate over ivermectin has come to be in the United States.
“There’s misinformation on both sides,” says Jennifer Granston, head of insights at Zignal Labs, a firm that conducts data analysis on internet trends. She cited inflated, unsubstantiated claims of both the drug’s efficacy and its harms. “At the end of the day, does this medication help COVID patients or does it not? That’s a scientific issue.”
How did a science question about the efficacy of an inexpensive, everyday drug become an inflamed public morality debate — where people on both sides believe the wrong position could cost lives? It’s a tale that spans science and politics, pitting health officials against celebrities and communal responsibilities against individual rights.
And it’s a debate that public health experts worry could prolong the pandemic as individuals forgo vaccines and proven prevention measures and instead take up alternative treatments that may not be effective.

Protesters for an anti-vaccine rally in Cincinnati in August carry a sign backing ivermectin. Belief in the drug’s efficacy often goes hand in hand with vaccine hesitancy.
Phil Didion/USA Today Network/Reuters
hide caption
toggle caption
Phil Didion/USA Today Network/Reuters

Protesters for an anti-vaccine rally in Cincinnati in August carry a sign backing ivermectin. Belief in the drug’s efficacy often goes hand in hand with vaccine hesitancy.
Phil Didion/USA Today Network/Reuters
Considering new uses for what advocates call a wonder drug
Advocates for ivermectin have called it a wonder drug — and it is, for treating parasites. In the 1970s, a team of researchers, headed by Kitasato Institute researcher Satoshi Omura and the drug company Merck, discovered a set of powerful anti-parasitic compounds in bacteria from a dirt sample dug up from a seaside golf course near Tokyo.
From that compound, Merck developed medicines that kill a wide range of parasites that plague animals and humans. Ivermectin, introduced in the early 1980s as a drug for livestock, became a blockbuster, making more than $1 billion in sales a year. The version of the drug launched for human use cured disfiguring parasitic infections such as elephantiasis and river blindness in developing countries. (It eradicated the latter in several countries.)
Omura and William Campbell, his counterpart at Merck, shared a Nobel Prize in 2015 for their discoveries related to the drug.
Early in the pandemic, given its track record, it seemed worth trying against COVID-19. In June 2020, a group of Australian researchers published a paper showing that large quantities of ivermectin could stop the coronavirus from replicating in cell cultures.
“But pretty quickly, people realized the problem with that was something called ‘pharmacokinetic mismatch,’ ” says Laurel Bristow, a science communicator and clinical research coordinator at Emory University. The amount of ivermectin a person would need to take to achieve that effect is up to 100 times the dose approved for humans. At that concentration, the drug might stop the virus — and may also harm the patient, she says.
The challenge for researchers has been to figure out whether a safe dose could be effective, Bristow says. Numerous studies have been published, and a few large trials are still underway.
Retracted studies and fights over evidence
Ivermectin research on COVID-19 published to date does not look promising, according to researchers who have closely considered the evidence.
“You have a large number of trials that have been done. Many of them are poorly done. They’re too small, they’re too short, they don’t measure the right things,” says Dr. Peter Lurie, president of the Center for Science in the Public Interest and a former associate commissioner at the Food and Drug Administration.
And at least two influential preprints that supported the use of ivermectin were later retracted when they were found to contain flawed or fabricated data.
Lurie and other health experts point to a review of the studies on ivermectin and COVID-19 published in the Cochrane Database of Systematic Reviews, considered to be the gold standard in assessing evidence on current medical topics. In reviewing the available research through May, the Cochrane researchers found “no evidence to support the use of ivermectin for treating or preventing COVID-19 infection,” though they acknowledged the data is limited.
Clinicians associated with a U.S. organization, the Front Line COVID-19 Critical Care Alliance, maintain there are dozens of studies that show a positive impact on COVID-19. But many of the studies they point to were omitted from the Cochrane analysis because the reviewers concluded their designs were faulty or drew on inaccurate comparisons.
“That doesn’t preclude the notion that the next clinical trial, if properly conducted, will not be one that actually demonstrates effectiveness,” Lurie says, “But at the moment, we can only work from what we currently know. And what we currently know is that there’s insufficient evidence to recommend this product at this time.”
Large, rigorous clinical trials are underway — including one in the U.K. run by Oxford University and an National Institutes of Health-funded study in the U.S. led by researchers at Duke University with multiple sites around the country. Emory researcher Bristow is lead coordinator for one of the study sites.
“People keep acting like there’s this huge censorship about ivermectin when really we’re actively working on figuring it out,” she says, “We’re trying to evaluate the potential efficacy of ivermectin for preventing hospitalization and relieving symptoms faster.”
Even if research showed an advantage to ivermectin, that wouldn’t make it a miracle COVID-19 cure, warns Aaron Friedberg, a primary care physician who supervises medical residents in the hospital at the Ohio State University Wexner Medical Center.
“Ultimately, when we’re talking about things being ‘effective,’ we just mean it works, even some,” he says, explaining that steroids are considered effective COVID-19 treatments in that they slightly increase the chances of survival among people treated properly with them.
Meanwhile, some people are overdosing on ivermectin. While the drug is generally considered to be safe in doses approved for human use, many who are taking it as an unproven treatment for COVID-19 are using more than the typically prescribed amount, says Michael Ganio of the American Society of Health-System Pharmacists, or using concentrated forms meant for livestock. And that has prompted warnings from U.S. federal agencies.
Bristow says the research community is devoting more time and resources to studying this drug, compared with other treatments, because of the immense interest around it. As was the case with hydroxychloroquine, though, she cautions that interest in the drug may be driven more by ideology than science.
A growing national passion for ivermectin
In May 2020, as the nation struggled to contain the coronavirus without a vaccine, then-President Donald Trump announced that he was taking hydroxychloroquine in an attempt to ward off infection despite warnings from the FDA. The idea that a cheap, widely available drug could end the pandemic provided an alternative solution for an administration struggling to contain the virus.
“It fits a political narrative, which is about reopening the economy as soon as possible,” says Yunkang Yang, a disinformation researcher at George Washington University, who recently co-authored a book chapter on how right-wing media and the Trump administration worked together to push hydroxychloroquine. “The miracle cure paints a rosy picture of the situation. It is portrayed as a quick fix that is designed to persuade people to go back to work.”
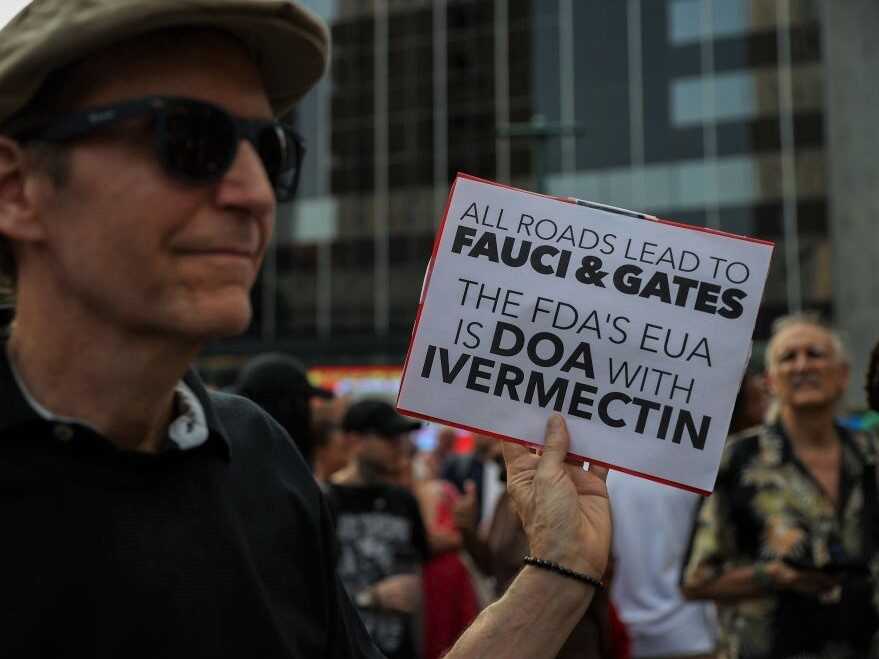
A protester at a September rally to protest vaccination mandates in New York City carries a sign supporting ivermectin.
Tayfun Coskun/Anadolu Agency via Getty Images
hide caption
toggle caption
Tayfun Coskun/Anadolu Agency via Getty Images

A protester at a September rally to protest vaccination mandates in New York City carries a sign supporting ivermectin.
Tayfun Coskun/Anadolu Agency via Getty Images
When COVID-19 vaccines arrived last winter, they relieved some of the pressure — but more Republicans were skeptical of the vaccines than Democrats, a divide that has only widened over time.
So the hunt for alternative cures continued to have political value. In December, Sen. Ron Johnson, R-Wis., invited Pierre Kory, a critical care physician then affiliated with St. Luke’s Aurora Medical Center in Milwaukee, to testify about ivermectin at a Senate committee hearing. Kory is a founding member and spokesperson for the Front Line COVID-19 Critical Care Alliance, a small group of doctors whose views on ivermectin diverge from the wider medical community.
At the Senate hearing, he stated that the drug was “proving to be of miraculous impact” and claimed unequivocally that it has a prophylactic effect against COVID-19: “It basically obliterates transmission of this virus. If you take it, you will not get sick,” he said.
Kory’s comments circulated widely on the internet but were not backed by solid scientific evidence available at the time or since. YouTube later removed videos of the hearing from their platforms, deeming it “inappropriate content,” but Kory’s championing of ivermectin had already received more than 1 million views, according to an Associated Press report.
The video’s removal led to cries of censorship from the right, weaving a thread of conspiracy through the narrative for those who were looking for it.
Soon right-wing media figures such as Fox News host Laura Ingraham began touting the drug. Other influencers such as comedian Joe Rogan also amplified the reputation of ivermectin — Rogan promoted the drug on his popular podcast and later announced he took it for COVID-19.
For people inclined to be suspicious of government scientists and federal policies on issues such as mask-wearing, ivermectin filled the place of the failed hydroxychloroquine as an alternative to the official federal guidance on how to prevent and treat COVID-19.
“It fits into the bigger narrative about the so-called ‘medical deep state’ [in which] scientists, pharmaceutical and political elites have an interest in making people use more expensive, experimental drugs” to increase the profits of the pharmaceutical industry, Yang says. “And they have an interest in not showing the public the cheap, widely available drugs that can supposedly cure COVID-19.” (Ingraham has labeled Dr. Anthony Fauci as part of the “medical deep state.”)

Ivermectin is an effective treatment for certain parasites in humans and animals, but there’s yet no clear evidence it helps treat COVID-19.
Mike Stewart/AP
hide caption
toggle caption
Mike Stewart/AP

Ivermectin is an effective treatment for certain parasites in humans and animals, but there’s yet no clear evidence it helps treat COVID-19.
Mike Stewart/AP
The toll of a misplaced faith
Midway through the summer, the delta variant started to burn through the United States. Cases exploded in places with low vaccination rates. In hot spots across the South and Midwest, worried people sometimes turned to the internet for answers.
Online mentions for ivermectin spiked: Seventy-four percent of the topic’s mentions for this year have taken place in the past two months, with a huge increase in August, Zignal’s analysis shows. “That’s where we’re really starting to see this story take off,” Zignal’s Granston says, “I’d also say that’s when we really start to see the story split.”
Rhetoric on both sides heated up. The Centers for Disease Control and Prevention, FDA and other public health agencies came out strongly against the use of the drug on the basis of the poor quality of evidence supporting it so far. Meanwhile, proponents of the “miracle cure” dug in, often citing the handful of medical experts affiliated with the Front Line COVID-19 Critical Care Alliance who defend it.
“Clear instances of disinformation are relatively easy to debunk,” Granston says. “The really hard stuff is where you have conflicting information. This is a very personal issue for people, because you’re talking about their health and everybody’s really grasping for answers. And that is outpacing the public health officials’ knowledge because the scientific studies haven’t been conducted on a broad scale yet.”
While those studies are underway, some people’s belief in ivermectin over other proven options, such as masks and vaccines, is giving them a false sense of security and control.
In some cases, the misinformation is actually killing them, says Kolina Koltai, a researcher who studies vaccine dissent at the University of Washington. Koltai likens vaccine refusal to not wearing a seat belt in a car because you heard of someone who survived an accident without a seat belt.
“If someone thinks they’re safe [because they’re taking ivermectin], they’re making a judgment that impacts not only their health but their community’s health,” she says, “by either use of resources at the hospital or [by getting and] spreading COVID. That is the real risk and danger of misinformation.”
The toll of COVID-19 on people who are unvaccinated has been harsh. By mid-September, as the delta variant continued to surge, hospitalizations were at their highest since early February; more than 1,800 people were dying of COVID-19 each day. The vast majority of people who have been hospitalized for or killed by the disease in recent months were not vaccinated.
Smith and her husband were among those who chose to forgo vaccination. Smith said she considered the vaccine to be “experimental,” according to a recording of a court hearing in the case shared with NPR by Ohio Capital Journal reporter Jake Zuckerman. “We didn’t feel confident that it had been out long enough,” Smith testified, “and weren’t sure of the damage that would ensue.”
Smith’s husband spent weeks on a ventilator in the ICU of a hospital near Cincinnati. On Aug. 23, a judge issued an emergency order to the hospital to begin administering 30 milligrams of ivermectin a day to the patient, as prescribed by a Front Line COVID-19 Critical Care Alliance doctor. On Sept. 6, a different judge reversed the ruling.
“Everyone involved wants Jeff Smith to get better,” Judge Michael Oster wrote in his decision. Still, after reviewing the evidence presented, the judge found “there can be no doubt that the medical and scientific communities do not support the use of ivermectin as a treatment for COVID-19.”
Doctors told the court that Jeffrey Smith’s condition had not improved since receiving ivermectin. But Julie Smith believed it had.
As of Sept. 18, Jeffrey Smith was still in the hospital on a ventilator, according to the couple’s lawyer, Ralph Lorigo.
The case mirrors the splintered conversations that are continuing to take place across the internet.
“It’s the perfect storm right now of something that is going to become a lot more complex and a lot more challenging,” Zignal’s Granston says, “There’s no clear side really winning out in this from what we can see.”



